Cranial Base Compression — a functional approach to leg pain
whole body posture!
A first-time neuromuscular therapy client came in for an initial visit this past week. Part of her issue stemmed from cranial base compression. It was an interesting presentation, and I thought it might be cool to share. I won’t share identifying information; none of the pictures you see here is my client.
Her current main concern is discomfort in her legs. She has had past neck and head issues, but they aren’t bothering her right now. She is quite aware of what’s going on in her body, has some training in a health-related field, and wants to get better.
We started with a postural assessment. “Oh good!” she said. “Nobody has done that yet.”
There were two clear patterns impacting her situation, and she could feel them when I brought them to her attention. Right now, I’m just going to talk about one. Her knee joints were hyperextended — the knee joints were behind her center of gravity line. That’s a problem. It’s an indicator of something “off,” a risk factor for future joint dysfunction, and part of her symptom picture.
A functional approach to resolving pain

with your head in this position?
Our bodies are very smart. If one major body part is *behind* the center of gravity, you can be pretty sure there is a compensating part somewhere up the chain, most likely *in front of* the center of gravity.
In my client’s case, her head and neck were forward. This is pretty common, especially for people who spend time on phones, computers, and such. Which is nearly all of us these days. Maybe even you?
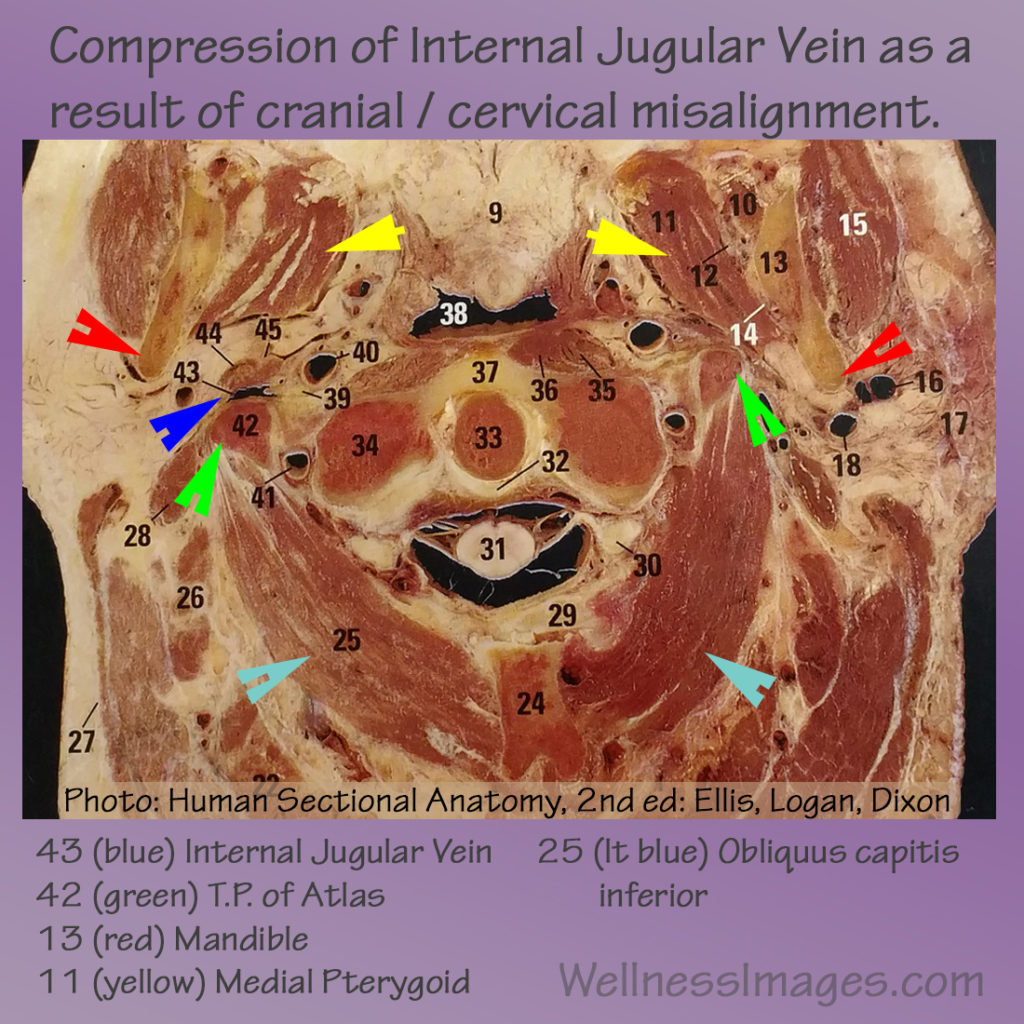
Compression in the lowest part of the back of the head can be part of the puzzle in this type of situation. It was for my new client. Where our head meets our neck. We refer to that as cranial base compression. It can also contribute to other issues, by the way: headaches, neck pain, back pain, dizziness, and so on. Depends on what else is going on for that person.
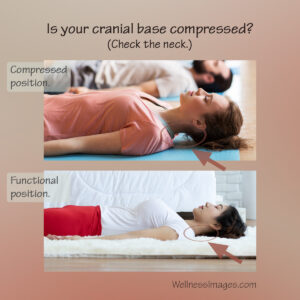
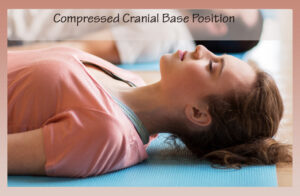
Let’s look at some pictures. See how this person’s chin is oriented “up” toward the ceiling and there’s lots of space between her neck and the floor?
And in the second picture, the person’s chin / head is more level. Her neck is much closer to the floor without a big gap. This orientation is our goal.

Cranial base compression and neck range of motion
When we first started the session, my client was unable to perform the motion of moving her neck back towards the flat surface she was lying on. She understood what I was asking her to do, she just couldn’t create the motion. I was confident she’d be able to get it back. As we worked and the compression began to decrease, she regained the ability to move her neck in that dimension. She was pretty excited!
So we continued to some other areas and ultimately finished up the session. How did this impact her main goal of more comfortable legs? Well, when she stood up after we were finished, I asked her to sense any differences in how she felt in terms of stability and balance.
She smiled & said, “My knees feel like they don’t extend back so much!” This was our goal! ![]()
The main thing we did in her session to impact that was address cranial base compression. Her head was less forward, and therefore her knees didn’t need to offset that balance as much. That will take stress off her leg muscles and knee / hip / ankle joints.
Assess. Find the reason. Help the body maintain balance.
See where I’m going with this? If we had not addressed that cranial base compression, any progress we made by working on her lower body / legs would have been short-lived, because we would have ignored the reason behind the muscle imbalance. This is an example of functional health care. One of our main goals is to restore proper function to the body, in as many domains as possible, so that its own wisdom will kick in and help the person maintain any changes we make.
There’s a bit more to to the story here, and so we will continue addressing some other factors in the coming weeks.
As a certified neuromuscular therapist since 1994, this is how I think. It applies to way more body variations than just compression of the cranial base. It’s the same type of thinking that goes into my functional health consulting work. Assess, and then address the reasons why the body is out of sorts — don’t just chase symptoms.
This particular situation is fairly easy to illustrate so you can see it. I hope you found the example helpful!
I am currently accepting new Neuromuscular Therapy clients. If you’re able to come for in-person appointments in my area (north central North Dakota) and would like to explore how this type of work might help you in your personal situation, feel free to email me: wellnessimages@gmail.com .